LOUISVILLE, Ky. – New research by the University of Louisville with colleagues at Harvard University could prevent dangerous and potentially life-threatening side effects from the delivery mechanism for targeted gene therapies meant to slow everything from muscle atrophy to vision loss.
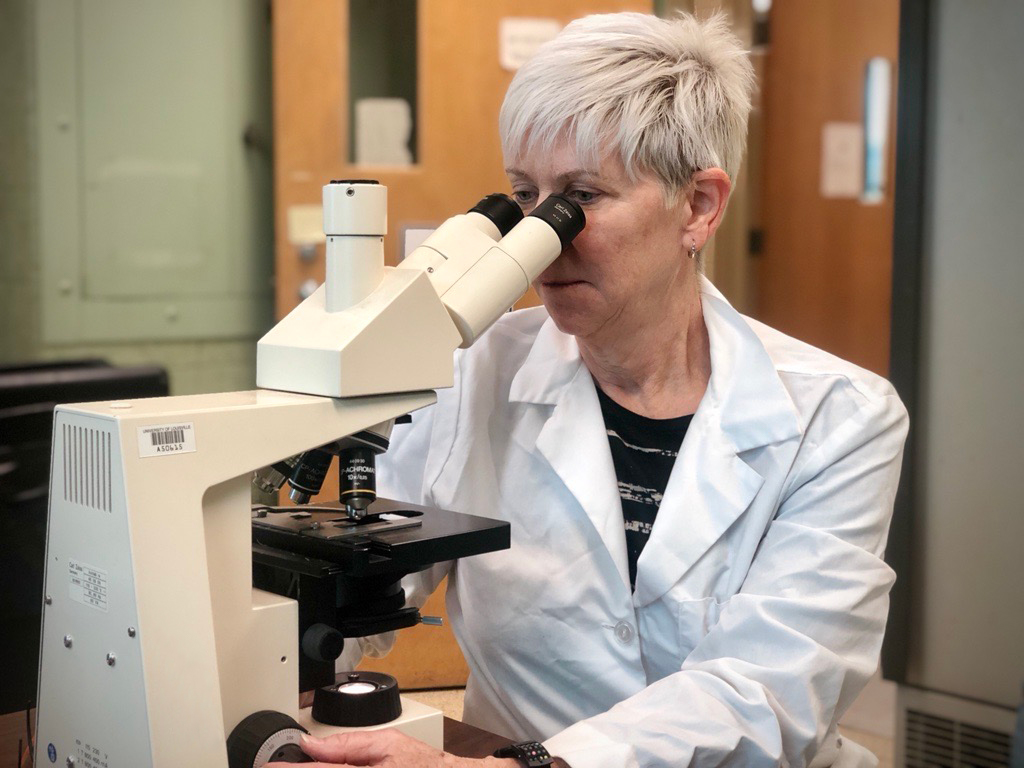
The work targets a leading delivery method for the therapies, adeno-associated virus (AAV), and recently was published in the journal Science Translational Medicine by UofL’s Maureen A. McCall, Ph.D., and her colleagues from Harvard University and its Wyss Institute.
AAV is used in treating a number of conditions, including the retinal diseases McCall studies at UofL. However, it also has been known to cause serious side effects, such as elevated immune response and inflammation.
“It’s a real problem since there’s no real control,” said McCall, the Kentucky Lions Eye Research Endowed Chair and a professor in the Departments of Ophthalmology and Visual Sciences and Anatomical Sciences and Neurobiology. “Even with the best-laid plans, you see some inflammatory retinal response, and the amount can vary widely, including dangerous levels.”
The new research focuses on the role of the viral capsid, a component in AAV that’s believed to cause this response. Parts of the viral capsid interact with a protein known as Toll-like receptor 9 (TLR9), which senses foreign DNA in the body. TLR9 triggers the immune response, which causes inflammation and can reduce or eliminate the therapy’s effects.
“So, the hypothesis was that if you could change that capsid code and mask it from the Toll-like receptor, that you could build a better delivery tool,” McCall said.
The idea is to “cloak” the deleterious part of the capsid with a series of synthetic DNA “inflammation-inhibiting oligonucleotide” sequences meant to stop TLR9’s reaction. In mouse models, the researchers saw a 95% reduction in inflammation.
In many cases, gene therapies for optical diseases are delivered through the retina since the blood-retina barrier helps to mitigate some of the immune response. Ying Kai Chan, Ph.D., a former postdoctoral fellow in George Church’s group at the Wyss Institute, reached out to McCall in 2018 to partner on this work because of her research expertise and the experience of her UofL colleagues with these injections, especially Wei Wang, M.D., Ph.D., assistant professor of ophthalmology.
McCall’s work at UofL specifically focuses on the use of gene therapies to treat retinal diseases, including retinitis pigmentosa and other conditions that eventually can cause blindness. For some of these conditions, there is no known cure and many therapies are still in development and clinical trials. McCall said eliminating side effects associated with AAV delivery gets researchers one step closer to successful treatment.
“Solving this key problem with delivery is huge,” she said. “These therapies show promise in significantly increasing people’s quality of life. My hope is that one day we can use these therapies to slow – or even stop – the progression of these diseases and restore sight.”
#WeAreUofL