Pancreatic cancer is one of the deadliest cancers, with a five-year survival rate of just 10% for patients diagnosed with pancreatic ductal adenocarcinoma (PDAC), the most common type. Further, one promising area of cancer treatment, immunotherapy, has not provided benefit for pancreatic cancer patients.
University of Louisville researchers recently have shown that beta-glucan, a natural carbohydrate, can generate enhanced immune responses to cancer in the pancreas and may lead to improved efficacy of immunotherapy for pancreatic cancer.
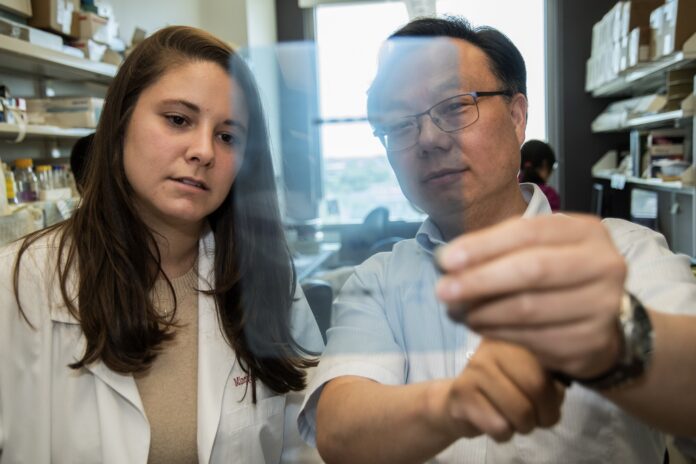
Jun Yan, chief of the Division of Immunotherapy in the Department of Surgery at UofL, said one of challenges for pancreatic cancer is that natural immune cells are unable to enter the pancreas to combat the growth of tumors, creating an immune desert.
“These tumors lack quality effector immune cells that can kill them,” Yan said. “In addition, pancreatic cancer has a unique tumor microenvironment that prevents the influx of anti-tumor immune cells.”
In new research published this month in Nature Communications, Anne Geller, an MD/PhD student, and a research team at UofL led by Yan demonstrate that a type of beta-glucan derived from yeast can alter the environment within the pancreas to promote anti-cancer immune cell migration to the site of the cancer. Beta-glucan, a naturally occurring carbohydrate found in plants, bacteria and fungi, is known to induce trained immunity, stimulating an immune response to a specific stimulus, such as pancreatic tumor cells.
Trained immunity is a new concept in the field of immunology and is the idea that innate immune cells possess a form of “memory,” which typically only has been considered to be a feature of adaptive immune cells such as T-cells. Using animal models, Yan and his team found that when they injected particulate beta-glucan into the peritoneal area, it accumulated in the pancreas and promoted anti-cancer immune cell migration to the area. These immune cells were found to have a trained immunity phenotype and effectively inhibited pancreatic cancer growth.
“This research demonstrates that a natural compound can stimulate trained immunity in pancreas,” Yan said.
The researchers also found that beta-glucan-stimulated trained immunity can enhance PD-1 antibody therapy in pancreatic cancer. Anti-PD-1 immunotherapy has been approved to treat many types of cancer including melanoma and lung cancer. However, this therapy has failed in treating pancreatic cancer. This research could be a breakthrough in successfully applying immunotherapy to pancreatic cancer.
“This research has a great potential for clinical translation as it elucidates a strategy for delivering therapeutics directly to the pancreas, identifies a mechanism of enhancing anti-tumor immune responses against pancreatic tumors and provides insight into ways of unleashing the awesome power of immunotherapies against PDAC,” Geller said. “This could be a breakthrough in treating the deadly cancer that has evaded so many other forms of treatment.”
Yan, director of the Immuno-Oncology Program at UofL Health – Brown Cancer Center and study coauthor, and surgical oncologist Robert C.G. Martin II are conducting a clinical trial using beta-glucan in pancreatc cancer patients as a proof-of-concept study.
“This publication demonstrates that a simple yeast-derived beta-glucan supplement has the potential to enhance a patient’s immune system and then respond more effectively to therapies in pancreatic cancer. The concept that patients’ immune systems can be ‘trained’ to see their pancreatic cancer as abnormal or foreign could be a crucial step in enhancing a patient’s overall survival and thus quality of life,” said Martin, professor and director of the UofL Division of Surgical Oncology and a co-author on the study.
According to the American Cancer Society, more than 60,000 adults are expected to be diagnosed with pancreatic cancer in the U.S. in 2022 and nearly 50,000 patients will die from the disease. Alex Trebek, long-time host of the game show “Jeopardy!” shared his pancreatic cancer diagnosis and treatment journey beginning in 2019. Trebek died in 2020, just over 18 months after announcing his diagnosis.
“UofL is committed to solving big, global challenges through research,” said Kevin Gardner, UofL’s executive vice president for research and innovation. “This work, leveraging the power of the immune system to better treat pancreatic cancer, could have a big impact in helping people live lives that are not just longer, but healthier and more resilient.”